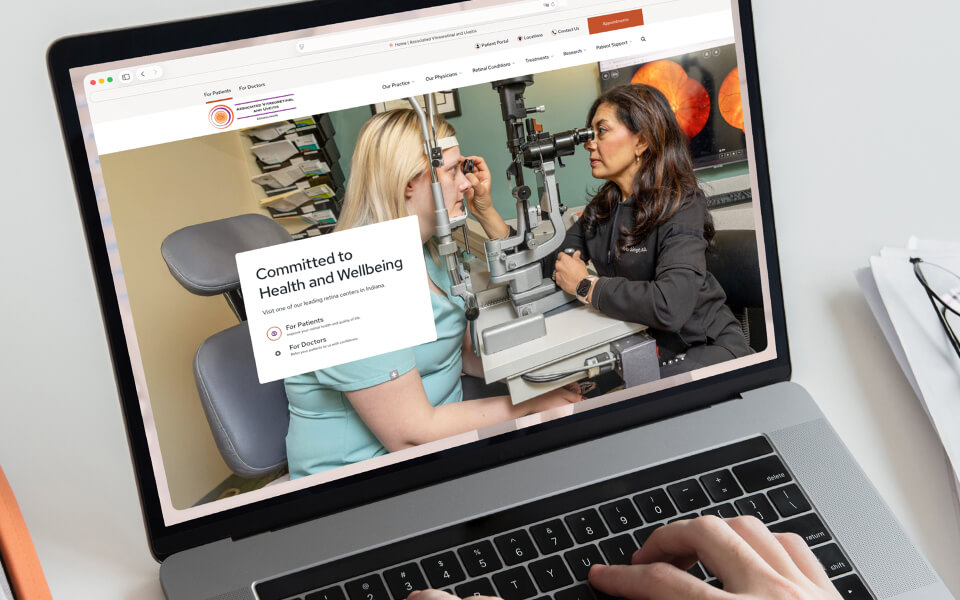
Welcome to the Associated Vitreoretinal and Uveitis Consultants of Indianapolis
We are dedicated to the enhancement and preservation of vision for patients with diseases of the retina, vitreous, and uvea. From four state-of-the-art offices in Indiana, our team provides comprehensive care of age-related macular degeneration, diabetic retinopathy, retinal detachment, inherited retinal disease, uveitis and many other retina-related eye diseases.
World-Class Retinal Care Near You
Our practice was founded in 1995 by Ramana Moorthy and James Fountain with the goal of providing world-class retina care to patients in central Indiana. Over the years, the practice has grown, but we continue to pride ourselves on delivering the best care with knowledge, skill, and compassion.
100+
Years of Combined Experience
10+
Clinical
Trials
7
Retina
Specialists
4
Convenient Locations
Memberships and Affiliations
“Excellent experience and would recommend to anybody without hesitation.”

“They really care about you and your vision.”
“Some of the most competent and compassionate doctors I have ever met.”

“Impressed by their expertise, efficiency, bedside manner, and compassion.”

Our Retina Specialists
Each of our highly-skilled retina specialists delivers focused, personalized care to patients every day while also participating in research and clinical trials to find new vision-saving treatments.
Ready to book an appointment?
Get started now.
Get started now.

A Holistic Approach to Patient Care
Our team understands that patients need comprehensive support beyond their medical treatments. From scheduling to billing to insurance navigation, you can count on us to make your experience here as stress-free and seamless as possible.

Research & Clinical Trials
Our physicians are actively engaged in clinical trials that help drive innovation and improve treatment options for patients in Delaware and nationwide. These trials not only pave the way for future medical breakthroughs but may also offer promising care alternatives for patients who qualify today. Learn more about our research program, and talk to your physician about our currently enrolling trials.

Specialized Care for Uveitis
If you’ve been diagnosed with uveitis — an umbrella term for inflammation within the eye — it’s important to receive care from someone with specialized training in the condition. Learn more about how our team can help treat and manage uveitis, working with you to achieve optimal outcomes.

Retina Consultants of America
Associated Vitreoretinal and Uveitis Consultants of Indianapolis is part of Retina Consultants of America (RCA), the largest retina care provider in the nation. Together, we're actively working to elevate patient experiences and advance treatment options through clinical trials.
Blog and News
Keep up with the latest news, updates, and announcements from our practice.